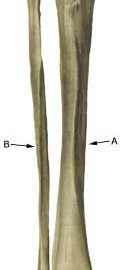
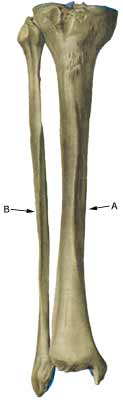
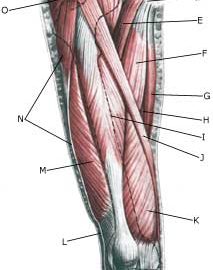
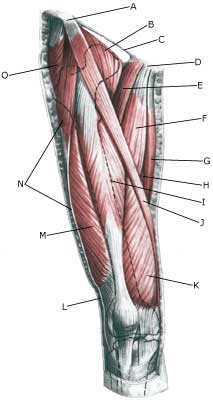
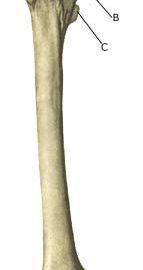
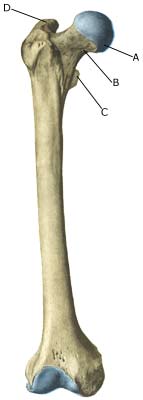
Cause: In cases of repeated uniform loads, a stress related inflammation, can occur where the muscle membrane fastens on the edge of the shin bone. The condition is most often seen in athletes who jump a lot and with frequent change of running surface or shoes. Symptoms: Pain upon applying pressure, particularly on the exterior edge of the shin bone and upon straining, and is aggravated when the foot is bent upwards against resistance (extension). Occasionally an irregular bone edge can be felt on the shin bone. Acute treatment: Examination: In light cases medical examination is not necessarily required. In cases with more pronounced pain or lack of progress despite relief, a medical examination is recommended to ensure the diagnosis and rule out amongst other things a stress fracture. A medical examination is usually sufficient in order to make the diagnosis. It can be necessary to supplement with X-ray, Scintigraphy, ultrasonography or MRI (article). Treatment: The treatment involves relief, stretching and slow rehabilitation. It is imperative that there are good shock absorbing soles in the shoes. Complications: If the course does not progress smoothly, you should be medically re-examined to ensure that the diagnosis is correct, and that complications have not arisen in the form of stress fracture. Special: Shock absorbing shoes or inlays will reduce the load. |