TRAINING LADDER FOR CHILDREN AND ADOLESCENTS:
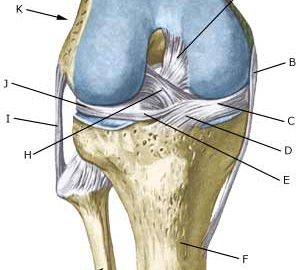
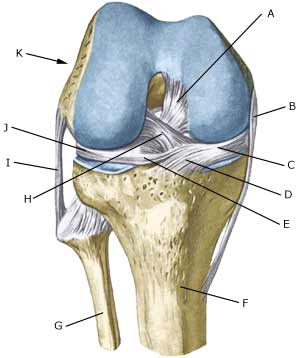
FOR RUPTURE OF THE POSTERIOR CRUCIATE LIGAMENT
(RUPTURA LIGAMENTUM CRUCIATUM POSTERIUS)
Uge 7-9 |
| The following exercises can only be considered as a supplement to the guidelines furnished by the doctor which performed the operation. Specific precautions are necessary as the operation can be complicated. The training must not bring about swelling or pain in the knee. | ||||||||||||||||||||||||||||||||||||||||||||||
| Unlimited: Cycling with raised saddle. Swimming. Running in deep water.
|
||||||||||||||||||||||||||||||||||||||||||||||
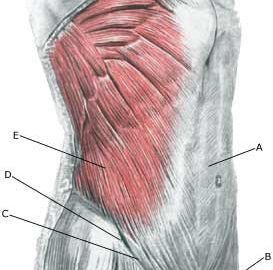
| Stretching is carried out in the following way: stretch the muscle group for 3-5 seconds. Relax for 3-5 seconds. The muscle group should subsequently be stretched for 20 seconds. The muscle is allowed to be tender, but must not hurt. Relax for 20 seconds, after which the procedure can be repeated.
The time consumed for stretching, coordination and strength training can be altered depending on the training opportunities available and individual requirements. |